Meniere's Disease
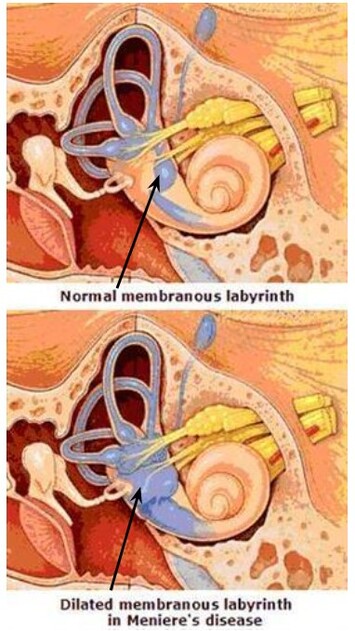
Ménière’s disease is a chronic “plumbing problem” of the inner ear (labyrinth). Fluid, called endolymph, housed in one of the inner ear chambers (the membranous labyrinth) collects in abnormally large amounts, causing swelling of that chamber and its membrane. Another chamber of the inner ear, called the bony labyrinth, houses a different fluid called perilymph. The membranous labyrinth is suspended within the perilymph of the bony labyrinth, resembling a tube within a tube. Both endolymph and perilymph contain sodium and potassium but in different ratios and, under normal conditions, do not mix.
Symptoms of a Ménière’s episode are triggered when the normal ratio of sodium and potassium becomes out of balance, resulting in inner ear swelling, potential microtears in the membranous labyrinth, and fluid leaking into the neighboring chamber, further disrupting the sensitive sodium-potassium ratios of each chamber.
The exact cause of Ménière’s disease is unknown, however it does appear to run in families, suggesting a genetic component. Other proposed causes include an autoimmune response, migraines, or circulatory problems. Meniere’s episodes may be triggered by stress, fatigue, pressure changes, dietary intake (particularly high sodium and low potassium), dehydration, caffeine, or alcohol. Some people may be sensitive to even subtle changes in sodium and potassium. Onset may also be trauma induced.
Ménière’s Disease affects 2 out of every 1000 people, and can begin at any age, although it is most common for the first episode to occur between age 40 and 60. The disease appears to “run its course” and resolve with age…something that actually improves with age! In the late stages of the disease, some may be afflicted with drop attacks, known as Tumarkin’s Otolithic Crisis. There is no loss of consciousness, purely a loss of vertical orientation lasting seconds. While these attacks are unpredictable, they are said to occur only in the late stage of the disease, signifying a means to an end.
A single episode may be referred to as Endolymphatic Hydrops. When the source appears to be trauma related, it is referred to as Traumatic Endolymphatic Hydrops. When symptoms are reoccurring, the condition is labeled as Ménière’s Disease. Classic Ménière’s Disease affects the entire inner ear, including the cochlea (hearing) and vestibule (balance). Less common, Ménière’s may affect only the balance portion (Vestibular Ménière’s) and even less common, may affect only the hearing portion (Cochlear Ménière’s). A more rare form of Ménière’s Disease is called Lermoyez’s Ménière Disease, in which hearing loss and tinnitus may precede the first attack of vertigo by months or years. In these cases, hearing may improve with the onset of vertigo. The only way to be certain of this rare form would be if you developed episodic vertigo in the future not caused by something else.
An episode of Ménière’s may last 20 minutes to 24 hours. The frequency of episodes varies widely. A typical episode may be preceded by a sensation of fullness in the diseased ear(s). A person may also notice changes in hearing or ringing in the ear(s) prior to an episode. During an episode, a person may experience severe vertigo (feeling of movement of self or environment without the presence of actual movement), imbalance, nausea and/or vomiting, aural fullness and changes in hearing. Oftentimes individuals feel very tired after an episode, requiring hours or a day to recover. In the beginning stages, most people will return to “normal” between episodes. Following a severe episode or repeated episodes, a person may have residual dizziness and instability and/or hearing impairment. In classic Ménière’s Disease, a low tone hearing loss is diagnosed. With repeated attacks, hearing loss can progress to all frequencies and become permanent.
Vestibular testing, to be performed with sophisticated equipment at specialized offices such as AVORA, is often indicated to assist in the diagnosis and to rule out other conditions. Less commonly performed or needed testing now available includes intratympanic GAD enhanced MRI (if no off-label issues) or intravenous GAD MRI but with delayed acquisition, allowing hydrops to be visualized in living subjects with either typical and atypical presentations as well as with symptomatic and, to a lesser extent, asymptomatic patients. Of interest, Ménière’s Disease is often over-diagnosed as the source of symptoms. A knowledgeable provider, especially when armed with proper testing equipment, can reduce the chances of misdiagnosis. Additionally, when a migraine component is present, Vestibular Migraines is more common compared to Ménière’s Disease.
Although there is no known cure for Ménière’s Disease, there are treatments that can help decrease the frequency and duration of episodes. While some medical professionals may say that diet has no impact, a low sodium diet is frequently prescribed to control the initial fluid build-up within the ear, which has been reported by the majority of patients to improve symptoms. Additional dietary recommendations include adequate hydration, proper intake of potassium, no caffeine, and reduced or no alcohol. A registered dietitian can help facilitate dietary changes to foster effective lifestyle choices. Additionally, specialized clinics, such as AVORA, can take the time to educate patients about the disease, available treatment options, and ways to minimize the effects of an episode and/or to reduce occurrences. Additionally, we can instruct in relaxation techniques, and aid in decreasing dizziness or balance impairments which may occur between episodes. Balance and vestibular exercises are not indicated when a person is symptom free between episodes. Additional non-pharmacological intervention may include psychology, tai chi, yoga, meditation or acupuncture to improve stress management. A medical doctor may prescribe medications to use during an attack to decrease symptoms of vertigo, nausea, and vomiting. If dietary and lifestyle changes are not enough to effectively manage symptoms, a medical doctor may prescribe a potassium sparing diuretic to help deplete your sodium while conserving your potassium. Conservative management is effective 60-80% of time. For those who do not respond to conservative treatment, a medical doctor (usually an Otolaryngologist, better known as ENT) may perform middle ear injections with a steroid as a first tier, gentamicin injections as a second tier, and surgical intervention as a last resort.
Symptoms of a Ménière’s episode are triggered when the normal ratio of sodium and potassium becomes out of balance, resulting in inner ear swelling, potential microtears in the membranous labyrinth, and fluid leaking into the neighboring chamber, further disrupting the sensitive sodium-potassium ratios of each chamber.
The exact cause of Ménière’s disease is unknown, however it does appear to run in families, suggesting a genetic component. Other proposed causes include an autoimmune response, migraines, or circulatory problems. Meniere’s episodes may be triggered by stress, fatigue, pressure changes, dietary intake (particularly high sodium and low potassium), dehydration, caffeine, or alcohol. Some people may be sensitive to even subtle changes in sodium and potassium. Onset may also be trauma induced.
Ménière’s Disease affects 2 out of every 1000 people, and can begin at any age, although it is most common for the first episode to occur between age 40 and 60. The disease appears to “run its course” and resolve with age…something that actually improves with age! In the late stages of the disease, some may be afflicted with drop attacks, known as Tumarkin’s Otolithic Crisis. There is no loss of consciousness, purely a loss of vertical orientation lasting seconds. While these attacks are unpredictable, they are said to occur only in the late stage of the disease, signifying a means to an end.
A single episode may be referred to as Endolymphatic Hydrops. When the source appears to be trauma related, it is referred to as Traumatic Endolymphatic Hydrops. When symptoms are reoccurring, the condition is labeled as Ménière’s Disease. Classic Ménière’s Disease affects the entire inner ear, including the cochlea (hearing) and vestibule (balance). Less common, Ménière’s may affect only the balance portion (Vestibular Ménière’s) and even less common, may affect only the hearing portion (Cochlear Ménière’s). A more rare form of Ménière’s Disease is called Lermoyez’s Ménière Disease, in which hearing loss and tinnitus may precede the first attack of vertigo by months or years. In these cases, hearing may improve with the onset of vertigo. The only way to be certain of this rare form would be if you developed episodic vertigo in the future not caused by something else.
An episode of Ménière’s may last 20 minutes to 24 hours. The frequency of episodes varies widely. A typical episode may be preceded by a sensation of fullness in the diseased ear(s). A person may also notice changes in hearing or ringing in the ear(s) prior to an episode. During an episode, a person may experience severe vertigo (feeling of movement of self or environment without the presence of actual movement), imbalance, nausea and/or vomiting, aural fullness and changes in hearing. Oftentimes individuals feel very tired after an episode, requiring hours or a day to recover. In the beginning stages, most people will return to “normal” between episodes. Following a severe episode or repeated episodes, a person may have residual dizziness and instability and/or hearing impairment. In classic Ménière’s Disease, a low tone hearing loss is diagnosed. With repeated attacks, hearing loss can progress to all frequencies and become permanent.
Vestibular testing, to be performed with sophisticated equipment at specialized offices such as AVORA, is often indicated to assist in the diagnosis and to rule out other conditions. Less commonly performed or needed testing now available includes intratympanic GAD enhanced MRI (if no off-label issues) or intravenous GAD MRI but with delayed acquisition, allowing hydrops to be visualized in living subjects with either typical and atypical presentations as well as with symptomatic and, to a lesser extent, asymptomatic patients. Of interest, Ménière’s Disease is often over-diagnosed as the source of symptoms. A knowledgeable provider, especially when armed with proper testing equipment, can reduce the chances of misdiagnosis. Additionally, when a migraine component is present, Vestibular Migraines is more common compared to Ménière’s Disease.
Although there is no known cure for Ménière’s Disease, there are treatments that can help decrease the frequency and duration of episodes. While some medical professionals may say that diet has no impact, a low sodium diet is frequently prescribed to control the initial fluid build-up within the ear, which has been reported by the majority of patients to improve symptoms. Additional dietary recommendations include adequate hydration, proper intake of potassium, no caffeine, and reduced or no alcohol. A registered dietitian can help facilitate dietary changes to foster effective lifestyle choices. Additionally, specialized clinics, such as AVORA, can take the time to educate patients about the disease, available treatment options, and ways to minimize the effects of an episode and/or to reduce occurrences. Additionally, we can instruct in relaxation techniques, and aid in decreasing dizziness or balance impairments which may occur between episodes. Balance and vestibular exercises are not indicated when a person is symptom free between episodes. Additional non-pharmacological intervention may include psychology, tai chi, yoga, meditation or acupuncture to improve stress management. A medical doctor may prescribe medications to use during an attack to decrease symptoms of vertigo, nausea, and vomiting. If dietary and lifestyle changes are not enough to effectively manage symptoms, a medical doctor may prescribe a potassium sparing diuretic to help deplete your sodium while conserving your potassium. Conservative management is effective 60-80% of time. For those who do not respond to conservative treatment, a medical doctor (usually an Otolaryngologist, better known as ENT) may perform middle ear injections with a steroid as a first tier, gentamicin injections as a second tier, and surgical intervention as a last resort.