The Peripheral Vestibular System
The vestibular system can be divided into two main systems; the central system (the brain and brainstem) and the peripheral system (the inner ear and the pathways to the brainstem). The inner ear, known as the labyrinth, contains 2 primary structures: the cochlea, responsible for hearing and the vestibular apparatus, responsible for maintaining balance, stability and spatial orientation.
The Anatomy of the Labyrinth (inner ear). In the image, the inner ear is in blue.
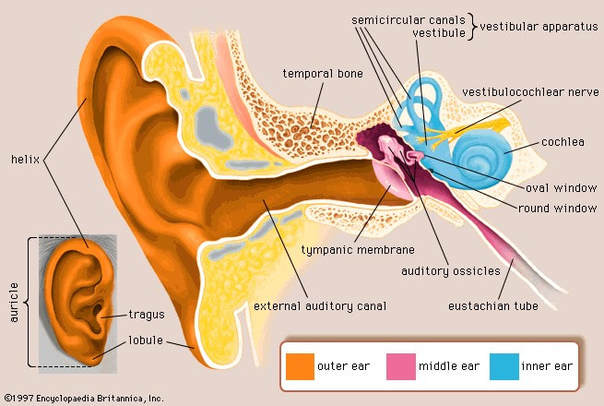
The labyrinth (inner ear marked as blue in the picture above) is encased in bone, called the bony labyrinth. Suspended by fluid (perilymph) within the bony labyrinth is another chamber called the membranous labyrinth, which contains its own fluid, called endolymph. Think of this as a hose within a hose, both filled with fluid. The fluid within the bony and membranous labyrinth both contain sodium and potassium, however, in different ratios. Conditions that affect the stability of these ratios, such as Meniere’s disease, can cause vertigo, dizziness, nausea, vomiting, ear fullness and tinnitus.
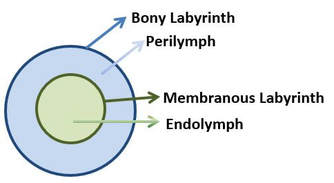
The Anatomy of the Vestibular System
The peripheral vestibular system (the non-auditory portion) has 3 semicircular canals that detect angular motion and 2 otolithic organs, the utricle and saccule, which collectively make up the vestibule and primarily detect linear motion.
The Otolithic Organs – the Utricle & the Saccule
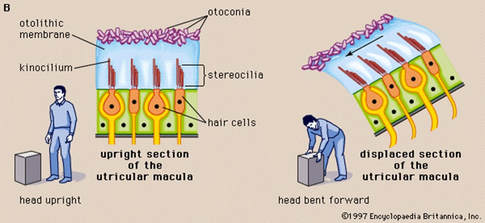
Collectively, the utricule and saccule make up the vestibule (see picture above). The utricle primarily detects linear motion in the horizontal plane (like a car moving forwards or backwards) while the saccule primarily detects motion in the vertical plane (like an elevator moving up or down). Each otolithic organ has hair cells embedded in a gelatinous material (like jelly or scoop of ice cream) with calcium carbonate crystals, called otoconia, attached to the surface. Imagine sprinkles on top of ice cream, with the sprinkles representing the otoconia (see picture to the right). Many refer to otoconia as “ear rocks” and is the substance responsible for a very common condition known as benign paroxysmal positional vertigo (BPPV) in which “ear rocks” fall off the “jelly” (sprinkles fall off the ice cream) and into one of the semicircular canals, causing vertigo, nausea and sometimes vomiting with changes in head position. The otoconia (ear rocks) serve a valuable purpose when they are in the correct locations within the utricle and saccule. They enable the otolithic organs to be sensitive to gravity (see picture above). For example, when you are in an elevator going up, you do not see the elevator moving and, although you are standing still, you know that you are going up! The otoconia allow you to sense that movement as long as there is a change in motion speed. When you take off, land, or hit turbulence in an airplane, you detect this motion because the otoconia are sensing the acceleration and deceleration. Once you are at cruising altitude while flying, you do not realize that you are traveling 500 miles per hour since there is no acceleration or deceleration.
Collectively, the utricule and saccule make up the vestibule (see picture above). The utricle primarily detects linear motion in the horizontal plane (like a car moving forwards or backwards) while the saccule primarily detects motion in the vertical plane (like an elevator moving up or down). Each otolithic organ has hair cells embedded in a gelatinous material (like jelly or scoop of ice cream) with calcium carbonate crystals, called otoconia, attached to the surface. Imagine sprinkles on top of ice cream, with the sprinkles representing the otoconia (see picture to the right). Many refer to otoconia as “ear rocks” and is the substance responsible for a very common condition known as benign paroxysmal positional vertigo (BPPV) in which “ear rocks” fall off the “jelly” (sprinkles fall off the ice cream) and into one of the semicircular canals, causing vertigo, nausea and sometimes vomiting with changes in head position. The otoconia (ear rocks) serve a valuable purpose when they are in the correct locations within the utricle and saccule. They enable the otolithic organs to be sensitive to gravity (see picture above). For example, when you are in an elevator going up, you do not see the elevator moving and, although you are standing still, you know that you are going up! The otoconia allow you to sense that movement as long as there is a change in motion speed. When you take off, land, or hit turbulence in an airplane, you detect this motion because the otoconia are sensing the acceleration and deceleration. Once you are at cruising altitude while flying, you do not realize that you are traveling 500 miles per hour since there is no acceleration or deceleration.
The Semicircular Canals
Unlike the otolithic organs, the semicircular canals are not sensitive to gravity since there are no otoconia normally in the canals. The 3 canals in each inner ear are oriented roughly 90 degrees to each other (like the corner of a room between 2 adjoining walls and the floor). Each semicircular canal has one bulbous shaped end called an ampulla. In the ampulla is a structure that is situated like a divider called the cupula (see picture below). In the cupula, there are multiple hair cells with bundles of hair that project up into the cupula. Within the hair bundles, there is one long hair called the kinocilium and many short hairs call the steriocilia. The cupula gets pushed or pulled during angular movement from the flow of endolymph causing the cupula to bend.
Unlike the otolithic organs, the semicircular canals are not sensitive to gravity since there are no otoconia normally in the canals. The 3 canals in each inner ear are oriented roughly 90 degrees to each other (like the corner of a room between 2 adjoining walls and the floor). Each semicircular canal has one bulbous shaped end called an ampulla. In the ampulla is a structure that is situated like a divider called the cupula (see picture below). In the cupula, there are multiple hair cells with bundles of hair that project up into the cupula. Within the hair bundles, there is one long hair called the kinocilium and many short hairs call the steriocilia. The cupula gets pushed or pulled during angular movement from the flow of endolymph causing the cupula to bend.
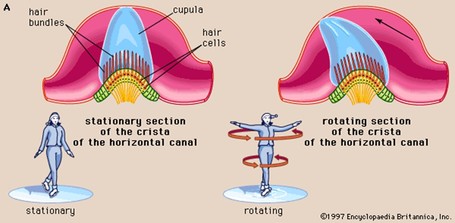
In response to the direction the cupula moves, the smaller hair cells (steriocilia) either move towards or away from the large hair cell (kinocilium). This information is converted into an electrical signal which ultimately produces corresponding eye movements.
The Vestibular Nerve
The inner ear has its own blood and nerve supply. The vestibulocochlear nerve (cranial nerve VIII) travels from the inner ear to the brainstem and is still considered part of the peripheral system until it enters the brainstem. The vestibular nerve has 2 portions; the superior vestibular nerve and the inferior vestibular nerve. Each portion attaches to specific structures in the inner ear (see diagram below).
The inner ear has its own blood and nerve supply. The vestibulocochlear nerve (cranial nerve VIII) travels from the inner ear to the brainstem and is still considered part of the peripheral system until it enters the brainstem. The vestibular nerve has 2 portions; the superior vestibular nerve and the inferior vestibular nerve. Each portion attaches to specific structures in the inner ear (see diagram below).
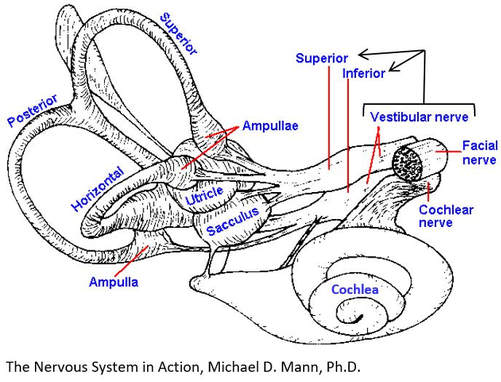
Vestibular disorders that damage one portion of the vestibular nerve most commonly affect the superior portion as it must travel through a narrower canal as compared to the inferior portion of the nerve. When the superior vestibular nerve is affected, it results in damage to the utricle, part of the saccule and the anterior (also called superior) and horizontal (also called lateral) canals. The posterior canal remains perfectly intact. In this scenario, it is then possible that when the utricule is damaged, otoconia (ear rocks within the utricle) fall off and drop into the posterior canal, resulting in BPPV in the posterior canal. This can be referred to as “the perfect storm” (a damaged system affecting an intact system causing it to also become dysfunctional). Some conditions will affect both portions of the vestibular nerve while still other conditions may affect both the vestibular and cochlear nerves, causing both hearing and balance problems simultaneously. You have 2 vestibular nerves, one from each ear, which must work together when sending signals to the brain. When one nerve’s signals are disrupted, this will immediately cause vertigo, dizziness, imbalance and often nausea and vomiting, which can last for several hours to several days until the brain learns how to reinterpret the signals. When the system does not “reset” on its own, vestibular rehabilitation helps to teach the system how to readapt and function. The blood supply follows a similar path as the nerve supply and, when compromised, will result in similar symptoms.
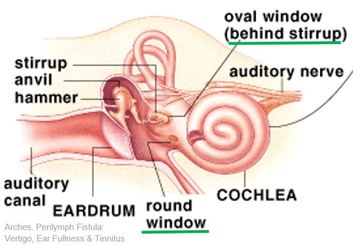
The final peripheral structures to briefly mention here are the oval window and round window, two openings from the middle ear to the inner ear, closed off by membranes (picture on left, underlined in green). They help to transmit sound. If these structures are compromised, allowing fluid to enter into the middle ear (known as a perilymphatic fistula) they may produce unwanted symptoms such as vertigo, imbalance, ear fullness, hearing loss, poor tolerance of loud sound, nausea and vomiting.
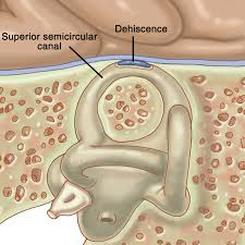
A third location where a fistula can occur is above the superior semicircular canal, in which the bone between the canal and the brain opens, known as a Superior Canal Dehiscence (SCD). Since the discovery of SCD, dehiscences have also been more recently discovered in the horizontal and posterior canals.
Psychological Connections
The pathways of the vestibular system overlap with pathways that are involved with anxiety, depression, migraines and pain (Balaban, 2013). Psychological conditions, when present prior to a vestibular disorder, may increase vestibular symptoms. Likewise, the onset of a vestibular disorder may cause psychological symptoms that were originally not present. Common complaints with many vestibular disorders are difficulty concentrating and paying attention, poor memory, increased dizziness with sound, light and busy environments, headaches and poor balance, along with increased or new anxiety or depression.
The pathways of the vestibular system overlap with pathways that are involved with anxiety, depression, migraines and pain (Balaban, 2013). Psychological conditions, when present prior to a vestibular disorder, may increase vestibular symptoms. Likewise, the onset of a vestibular disorder may cause psychological symptoms that were originally not present. Common complaints with many vestibular disorders are difficulty concentrating and paying attention, poor memory, increased dizziness with sound, light and busy environments, headaches and poor balance, along with increased or new anxiety or depression.
The Function of the Peripheral Vestibular System
As previously mentioned, the vestibular system is responsible for maintaining balance, stability and spatial orientation. There are several reflexes responsible for these responses. Similar to tapping your knee with a reflex hammer and your leg extending out, there are responses that occur with movement to keep your vision and body stable.
Vestibular Ocular Reflex (VOR): is a reflex that coordinates eye and head movement in order to keep an object in focus. The VOR is one of the fastest reflexes in the human body. Head movement must be compensated for almost immediately by the eyes in order to have clear vision. This means when your head moves one direction, your eyes must move in an equal and opposite direction at virtually the same speed to keep a target in focus. For example, when you are walking your head is not staying perfectly still, moving side to side and up and down as you walk, yet objects don’t sway or jump up and down (if the VOR is working properly). The VOR is triggering your eyes to move in the opposite direction of your head to keep objects in focus. If the VOR is deficient, you may experience oscillopsia (objects appear to blur or jump) when you are in motion. Your VOR works best at frequencies greater than 1 Hz, which is equivalent to turning your head to the right and then the left in one second. If your head is moving slower than 1 Hz, your visual system will take over the responsibilities. Routine daily activities generally range between less than 1 Hz to about 4 Hz, while walking averages between 2 to 4 Hz. Running may challenge the system up towards 10 Hz or greater depending on speed and terrain. Testing the VOR involves fast head movement while looking at a fixed target, known as a Head Thrust Test or Head Impulse Test. When done manually by a provider, the provider is looking for a delayed response in the eyes. A more sophisticated way of testing the VOR is called video head impulse testing or vHIT for short. It uses special infrared goggles and a computer to analyze results more precisely and to pick up deficiencies that are not visible to the human eye. It tests all 6 canals, the first test of its kind. The equipment is only recently available and still quite expensive so it is only found in limited locations.
Vestibular Collic Reflex (VCR): A reflex that, in response to information from the otolithic organs and semicircular canals, activates neck musculature to stabilize the head. We do not currently have a controlled way to test this reflex as the pathway is not fully understood.
Vestibular Spinal Reflex (VSR): is a reflex that maintains your posture and stabilizes your body to maintain an upright position. It refers to reactions that happen below the neck, such as staying on a bucking bull. Through a serious of events, an impulse is sent to your spinal cord to active muscles to keep you upright.
For example, if you are falling forward, the muscles on the back side of your body contract (pull) while the muscles on the front side of your body elongate (push) in an attempt to bring you back to center. If someone bumps into you on the right and you start falling to the left, you need muscles on both sides of your body to activate (a push from one side and a pull from the other) so that you don’t fall down.
Advanced Testing
Recall that the 3 semicircular canals sense angular motion and the 2 otolithic organs sense primarily linear motion relative to gravity. In part, these structures can be tested without sophisticated equipment if you have a knowledgeable provider who understands what they are looking for. However, the system is tested in more detail and specificity when sophisticated equipment is available. Infrared Video Frenzel Goggles allow for observing the eyes in the dark (without the patient focusing on a target), enlarge the eyes on a screen for easier viewing and records the eye movements for repeated playback. VNG (videonystagmography) software converts eye movements into a computer generated signal, also increasing the likelihood of an accurate diagnosis. Video Head Impulse testing (vHIT or vHIMP), which tests all 6 canals, and Suppression Head Impulse (SHIMP) testing, which looks at the amount of residual function in the horizontal canals, also help to isolate and quantify the source and extent of the problem, respectively. As with most vestibular equipment, this equipment is expensive and found in limited locations, usually clinics which specialize in vestibular testing and treatment. Other computerized testing exists to test other portions of the vestibular system or to confirm a suspected diagnosis such as caloric testing (which tests only the horizontal canals at a very slow frequency), VEMP (vestibular evoked myogenic potential) testing and rotary chair testing (prior hallmark testing to confirm a bilateral (both sides) vestibular loss before the availability of vHIMP & SHIMP testing, which not only will identify a bilateral vestibular loss but will also determine which of the 6 canals are affects (rotary chair only assess the horizontal canals) and how much, if any, vestibular function remains in the horizontal canals).
Summary
Since there are direct connections from the inner ears to the eyes and brain, injuries or deficiencies in any number of these structures can produce dysfunction in balance, hearing and abnormal eye movements. Testing exists to evaluate the response of the eyes in order to determine if there is dysfunction in the peripheral, central or both vestibular systems.
Author: Kim Fox, DPT
Sources
Childs L. Assessing vestibular dysfunction. Exploring treatments of a complex condition. Rehab Management [serial online]. July 2010;23(6):24-25.
Hain, Timothy, MD. “Postural, Vestibulospinal and Vestibulocollic Reflexes” Dizziness-and-balance.com. Timothy Hain, MD, Last modified March 3, 2014. Accessed July 5, 2014. http://www.dizziness-and-balance.com/anatomy/vspine.htm
Mann, Michael, PhD. “The Nervous System in Action” Chapter 9. Accessed online July 5, 2014. http://michaeldmann.nett/mann9.html
Balaban, Carrey, PhD. “A Neurophysiologic Explanation of Illness Behaviors Commonly Seen in Persons with Vestibular Disorders.” Vestibular Rehabilitation: An Advanced Course & Update. University of Pittsburgh. Volume 1. May 17-19, 2013.
As previously mentioned, the vestibular system is responsible for maintaining balance, stability and spatial orientation. There are several reflexes responsible for these responses. Similar to tapping your knee with a reflex hammer and your leg extending out, there are responses that occur with movement to keep your vision and body stable.
Vestibular Ocular Reflex (VOR): is a reflex that coordinates eye and head movement in order to keep an object in focus. The VOR is one of the fastest reflexes in the human body. Head movement must be compensated for almost immediately by the eyes in order to have clear vision. This means when your head moves one direction, your eyes must move in an equal and opposite direction at virtually the same speed to keep a target in focus. For example, when you are walking your head is not staying perfectly still, moving side to side and up and down as you walk, yet objects don’t sway or jump up and down (if the VOR is working properly). The VOR is triggering your eyes to move in the opposite direction of your head to keep objects in focus. If the VOR is deficient, you may experience oscillopsia (objects appear to blur or jump) when you are in motion. Your VOR works best at frequencies greater than 1 Hz, which is equivalent to turning your head to the right and then the left in one second. If your head is moving slower than 1 Hz, your visual system will take over the responsibilities. Routine daily activities generally range between less than 1 Hz to about 4 Hz, while walking averages between 2 to 4 Hz. Running may challenge the system up towards 10 Hz or greater depending on speed and terrain. Testing the VOR involves fast head movement while looking at a fixed target, known as a Head Thrust Test or Head Impulse Test. When done manually by a provider, the provider is looking for a delayed response in the eyes. A more sophisticated way of testing the VOR is called video head impulse testing or vHIT for short. It uses special infrared goggles and a computer to analyze results more precisely and to pick up deficiencies that are not visible to the human eye. It tests all 6 canals, the first test of its kind. The equipment is only recently available and still quite expensive so it is only found in limited locations.
Vestibular Collic Reflex (VCR): A reflex that, in response to information from the otolithic organs and semicircular canals, activates neck musculature to stabilize the head. We do not currently have a controlled way to test this reflex as the pathway is not fully understood.
Vestibular Spinal Reflex (VSR): is a reflex that maintains your posture and stabilizes your body to maintain an upright position. It refers to reactions that happen below the neck, such as staying on a bucking bull. Through a serious of events, an impulse is sent to your spinal cord to active muscles to keep you upright.
For example, if you are falling forward, the muscles on the back side of your body contract (pull) while the muscles on the front side of your body elongate (push) in an attempt to bring you back to center. If someone bumps into you on the right and you start falling to the left, you need muscles on both sides of your body to activate (a push from one side and a pull from the other) so that you don’t fall down.
Advanced Testing
Recall that the 3 semicircular canals sense angular motion and the 2 otolithic organs sense primarily linear motion relative to gravity. In part, these structures can be tested without sophisticated equipment if you have a knowledgeable provider who understands what they are looking for. However, the system is tested in more detail and specificity when sophisticated equipment is available. Infrared Video Frenzel Goggles allow for observing the eyes in the dark (without the patient focusing on a target), enlarge the eyes on a screen for easier viewing and records the eye movements for repeated playback. VNG (videonystagmography) software converts eye movements into a computer generated signal, also increasing the likelihood of an accurate diagnosis. Video Head Impulse testing (vHIT or vHIMP), which tests all 6 canals, and Suppression Head Impulse (SHIMP) testing, which looks at the amount of residual function in the horizontal canals, also help to isolate and quantify the source and extent of the problem, respectively. As with most vestibular equipment, this equipment is expensive and found in limited locations, usually clinics which specialize in vestibular testing and treatment. Other computerized testing exists to test other portions of the vestibular system or to confirm a suspected diagnosis such as caloric testing (which tests only the horizontal canals at a very slow frequency), VEMP (vestibular evoked myogenic potential) testing and rotary chair testing (prior hallmark testing to confirm a bilateral (both sides) vestibular loss before the availability of vHIMP & SHIMP testing, which not only will identify a bilateral vestibular loss but will also determine which of the 6 canals are affects (rotary chair only assess the horizontal canals) and how much, if any, vestibular function remains in the horizontal canals).
Summary
Since there are direct connections from the inner ears to the eyes and brain, injuries or deficiencies in any number of these structures can produce dysfunction in balance, hearing and abnormal eye movements. Testing exists to evaluate the response of the eyes in order to determine if there is dysfunction in the peripheral, central or both vestibular systems.
Author: Kim Fox, DPT
Sources
Childs L. Assessing vestibular dysfunction. Exploring treatments of a complex condition. Rehab Management [serial online]. July 2010;23(6):24-25.
Hain, Timothy, MD. “Postural, Vestibulospinal and Vestibulocollic Reflexes” Dizziness-and-balance.com. Timothy Hain, MD, Last modified March 3, 2014. Accessed July 5, 2014. http://www.dizziness-and-balance.com/anatomy/vspine.htm
Mann, Michael, PhD. “The Nervous System in Action” Chapter 9. Accessed online July 5, 2014. http://michaeldmann.nett/mann9.html
Balaban, Carrey, PhD. “A Neurophysiologic Explanation of Illness Behaviors Commonly Seen in Persons with Vestibular Disorders.” Vestibular Rehabilitation: An Advanced Course & Update. University of Pittsburgh. Volume 1. May 17-19, 2013.